Main criterionhigh blood pressure (or high blood pressure)as a whole group of diseases - stable, that is, detected by repeated measurements on different days, an increase in blood pressure (BP).The question of what type of blood pressure is considered high is not as simple as it seems.The fact is that in practically healthy people the range of blood pressure values is quite wide.The results of long-term observation of people with different levels of blood pressure showed that starting from the level of 115/75 mm Hg. Art., each additional increase in blood pressure by 10 mm Hg. Art.is accompanied by an increased risk of developing cardiovascular diseases (mainly coronary heart disease and stroke).However, the benefits of modern methods of treating high blood pressure have been proven mainly only for patients whose blood pressure exceeded 140/90 mm Hg. Art.It is for this reason that it was agreed to consider this threshold value as a criterion for identifying high blood pressure.
Increased blood pressure can be accompanied by dozens of different chronic diseases, and hypertension is only one of them, but the most common: about 9 out of 10 cases. The diagnosis of hypertension is established in cases where there is a stable increase in blood pressure, but no other diseases leading to an increase in blood pressure are detected.
Hypertension is a disease whose main manifestation is a stable increase in blood pressure.Risk factors that increase the likelihood of its development have been established through observation of large groups of people.In addition to some people's genetic predisposition, these risk factors include:
- obesity;
- inactivity;
- excessive consumption of table salt, alcohol;
- chronic stress;
- smoking.
In general, all these characteristics that accompany the modern urban lifestyle in industrialized countries.This is why hypertension is considered a lifestyle disease, and targeted changes for the better should always be considered as part of a hypertension treatment program on a case-by-case basis.
What other diseases are accompanied by increased blood pressure?These include many kidney diseases (pyelonephritis, glomerulonephritis, polycystic disease, diabetic nephropathy, stenosis (narrowing) of the renal arteries, etc.), a number of endocrine diseases (adrenal tumors, hyperthyroidism, Cushing's disease and syndrome), obstructive sleep apnea syndrome and some other rarer diseases.Regular use of medications such as glucocorticosteroids, nonsteroidal anti-inflammatory drugs, and oral contraceptives can also lead to persistent increases in blood pressure.The diseases and conditions listed above lead to the development of so-called secondary or symptomatic hypertension.The doctor makes a diagnosis of hypertension if, during a conversation with the patient, checking the history of the disease, an examination, as well as based on the results of some, mostly simple, laboratory and instrumental research methods, the diagnosis of secondary arterial hypertension seems unlikely.
If you notice similar symptoms, consult your doctor.Do not treat yourself, it is dangerous for your health!
Symptoms of high blood pressure
For many people, high blood pressure itself does not manifest itself in any subjective sensations.If high blood pressure is accompanied by symptoms, this may include a feeling of heaviness in the head, headache, blinking in the eyes, nausea, dizziness, unsteadiness when walking, as well as a number of other symptoms that are rather non-specific to high blood pressure.The symptoms listed above are manifested much more clearly during a hypertensive crisis - a sudden significant increase in blood pressure, leading to a sharp deterioration in condition and well-being.
It would be possible to continue listing possible symptoms of hypertension, separated by commas, but this does not bring any particular benefit.For what?Firstly, all these symptoms are not specific for hypertension (that is, they can occur individually or in various combinations in other diseases), and secondly, to establish the presence of high blood pressure, the very fact of a stable increase in blood pressure is important.And this is not revealed by the assessment of subjective symptoms, but only by measuring blood pressure, and this repeatedly.This means, firstly, that "in one session" one should measure blood pressure two or three times (with a short break between measurements) and take the arithmetic average of two or three measured values as the true blood pressure.Secondly, the stability of the increase in blood pressure (diagnostic criterion for hypertension as a chronic disease) should be confirmed by measurements on different days, preferably with an interval of at least a week.
If a hypertensive crisis develops, there will certainly be symptoms, otherwise it is not a hypertensive crisis, but simply an asymptomatic increase in blood pressure.And these symptoms can be either those listed above, or other, more serious ones - they are discussed in the "Complications" section.
Symptomatic (secondary) arterial hypertension develops in the context of other diseases, and therefore their manifestations, in addition to the actual symptoms of arterial hypertension (if any), depend on the underlying disease.For example, with hyperaldosteronism, this can be muscle weakness, cramps and even temporary paralysis (lasting hours or days) of the muscles of the legs, arms and neck.With obstructive sleep apnea syndrome - snoring, sleep apnea, daytime sleepiness.

If hypertension over time - usually many years - leads to damage to various organs (in this context they are called "target organs"), then this can manifest itself in a decrease in memory and intelligence, stroke or transient stroke, an increase in the thickness of the walls of the heart, accelerated development of atherosclerotic plaques in the vessels of the heart and other organs, myocardial infarction or angina, a decrease in the rate ofblood filtration in the kidneys, etc.the manifestations will be caused by these complications, and not by an increase in blood pressure per se.
Pathogenesis of arterial hypertension
In hypertension, dysregulation of vascular tone and increased blood pressure are the main content of this disease, so to speak, its “quintessence”.Factors such as genetic predisposition, obesity, inactivity, excessive consumption of table salt, alcohol, chronic stress, smoking and many others, mainly related to lifestyle characteristics, over time lead to a disruption in the functioning of the endothelium - the inner layer of arterial vessels of a cell layer thick, which actively participates in the regulation of tone, and therefore the lumen of blood vessels.The tone of microvascular vessels, and therefore the volume of local blood flow in organs and tissues, is regulated autonomously by the endothelium and not directly by the central nervous system.This is a local blood pressure regulation system.However, there are other levels of blood pressure regulation - the central nervous system, the endocrine system and the kidneys (which also achieve their regulatory role largely through their ability to participate in hormonal regulation at the level of the entire organism).Violations of these complex regulatory mechanisms lead, in general, to a decrease in the ability of the entire system to finely adapt to the constantly changing needs of organs and tissues for blood supply.
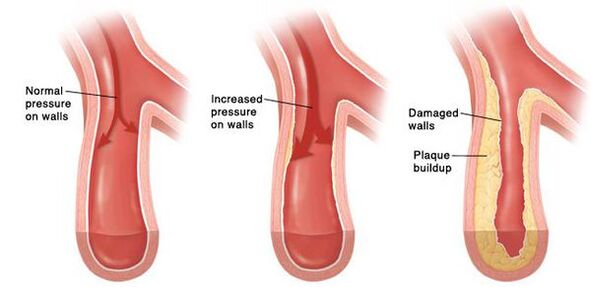
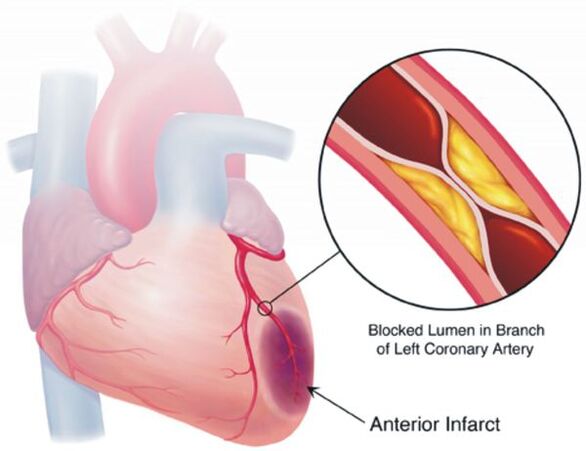
Over time, a persistent spasm of small arteries develops, and subsequently their walls change so much that they are no longer able to return to their original state.In larger vessels, due to constantly high blood pressure, atherosclerosis develops at an accelerated rate.The walls of the heart thicken, myocardial hypertrophy develops, then expansion of the cavities of the left atrium and left ventricle.Increased pressure damages the glomeruli, their number decreases, and as a result, the ability of the kidneys to filter blood decreases.In the brain, due to changes in the blood vessels supplying it, negative changes also occur - small foci of hemorrhages appear, as well as small areas of necrosis (death) of brain cells.When an atherosclerotic plaque ruptures into a sufficiently large vessel, thrombosis occurs, the lumen of the vessel is blocked, which leads to a stroke.
Classification and stages of development of arterial hypertension
Hypertension, depending on the magnitude of high blood pressure, is divided into three degrees.In addition, taking into account the increase in the risk of cardiovascular diseases on a “year-decade” scale, from a blood pressure level above 115/75 mm Hg. Art., there are several other gradations of blood pressure levels.
If the values of systolic and diastolic blood pressure belong to different categories, the degree of high blood pressure is assessed by the higher of the two values, and it does not matter - systolic or diastolic.The degree of increase in blood pressure when diagnosing hypertension is determined by repeated measurements on different days.
In some countries, the stages of hypertension continue to be distinguished, while the European guidelines for the diagnosis and treatment of high blood pressure do not mention any stages.The identification of stages aims to reflect the progressive evolution of hypertension from its onset to the appearance of complications.
There are three steps:
- Stage Iimplies that there is still no obvious damage to the organs that are most often affected by this disease: there is no hypertrophy (hypertrophy) of the left ventricle of the heart, there is no significant decrease in the filtration rate in the kidneys, which is determined taking into account the level of creatinine in the blood, albumin protein is not detected in urine, thickening of the walls of the carotid arteries or plaquesof atherosclerosis in these are not detected, etc.asymptomatic.
- If there is at least one of the listed signs, diagnoseStage IIhypertension.
- Finally, aboutStage IIIHypertension is said when there is at least one cardiovascular disease with clinical manifestations associated with atherosclerosis (myocardial infarction, stroke, angina pectoris, atherosclerotic lesion of the arteries of the lower extremities), or, for example, severe kidney damage, manifested by a pronounced decrease in filtration and/or significant loss of protein in urine.
These stages do not always replace each other naturally: for example, a person suffered a myocardial infarction and after a few years an increase in blood pressure occurred - it turns out that such a patient immediately suffers from stage III hypertension.The purpose of staging is primarily to classify patients according to their risk of cardiovascular complications.Therapeutic measures also depend on this: the higher the risk, the more intensive the treatment.When formulating a diagnosis, risk is assessed according to four gradations.At the same time, the 4th gradation corresponds to the greatest risk.
Complications of high blood pressure
The goal of treating hypertension is not to “lower” high blood pressure, but to minimize the risk of cardiovascular and other long-term complications, since this risk – again, when assessed on a “year-decade” scale – increases for each additional 10 mm Hg.Art.already from a blood pressure level of 115/75 mm Hg. Art.These are complications such as stroke, coronary heart disease, vascular dementia (dementia), chronic renal failure and chronic heart failure, atherosclerotic vascular lesions of the lower extremities.
Most patients with hypertension do not worry about anything at the moment, so they do not have much motivation to seek treatment, regularly take a certain minimum of medications and change their lifestyle to a healthier one.However, in the treatment of hypertension, there are no one-time measures that would allow you to forget about this disease forever without doing anything else to treat it.
Diagnosis of high blood pressure
With the diagnosis of arterial hypertension as such, everything is usually quite simple: this requires only repeatedly recorded blood pressure at the level of 140/90 mm Hg. Art.and higher.But hypertension and high blood pressure are not the same thing: as already mentioned, increased blood pressure can manifest itself in a number of diseases, and hypertension is only one of them, although the most common.When making a diagnosis, the doctor must, on the one hand, ensure that the increase in blood pressure is stable and, on the other hand, assess the likelihood that the increase in blood pressure is a manifestation of symptomatic (secondary) hypertension.
To do this, at the first stage of diagnostic research, the doctor finds out at what age blood pressure began to increase, whether there are symptoms such as, for example,snoring with pauses in breathing during sleep, attacks of muscle weakness, unusual impurities in urine, attacks of sharp heartbeat with sweating and headaches, etc.It makes sense to specify which medications and dietary supplements the patient is taking, because in some cases they can cause an increase in blood pressure or a worsening of already high blood pressure.Several routine diagnostic tests (performed in almost all patients with high blood pressure), as well as information obtained during an interview with a doctor, make it possible to assess the likelihood of certain forms of secondary hypertension: a complete urinalysis, determination of blood concentrations of creatinine and glucose, and sometimes potassium and other electrolytes.In general, taking into account the low prevalence of secondary forms of arterial hypertension (about 10% of all cases), the continued search for these diseases as a possible cause of arterial hypertension must have good reasons.Therefore, if at the first stage of diagnostic research no significant data are found in favor of the secondary nature of arterial hypertension, in the future it is considered that blood pressure is increased due to hypertension.This judgment may sometimes be revised later as new data about the patient becomes available.
In addition to looking for data on the possible secondary nature of increased blood pressure, the doctor determines the presence of risk factors for cardiovascular diseases (this is necessary for assessing the prognosis and a more targeted search for damage to internal organs), as well as, possibly, pre-existing diseases of the cardiovascular system or their asymptomatic lesions - this affects the assessment of the prognosis and stage of hypertension, the choice of therapeutic measures.For this purpose, in addition to talking with the patient and examining him, a number of diagnostic studies are carried out (for example, electrocardiography, echocardiography, ultrasound of the neck vessels and, if necessary, some other studies, the nature of which is determined by the medical data already obtained about the patient).

Daily monitoring of blood pressure using special compact devices allows you to assess changes in blood pressure during the patient's usual lifestyle.This study is not necessary in all cases - especially if blood pressure measured during a doctor's appointment differs significantly from that measured at home, if it is necessary to assess nighttime blood pressure, if episodes of hypotension are suspected, and sometimes to assess the effectiveness of treatment.
So, certain diagnostic methods when examining a patient with arterial hypertension are used in all cases;the use of other methods is more selective, based on the data already obtained on the patient, to verify the assumptions made by the doctor during the preliminary examination.
Treatment of high blood pressure
As for non-drug measures aimed at treating hypertension, the most convincing evidence has accumulated on the positive role of reducing salt intake, reducing and maintaining body weight at this level, regular physical exercise (effort), moderate alcohol consumption, as well as increasing the content of vegetables and fruits in the diet.Only all these measures are effective within the framework of long-term changes in the unhealthy lifestyle that led to the development of hypertension.For example, a 5 kg decrease in body weight resulted in a decrease in blood pressure of 4.4/3.6 mmHg on average.Art.- it doesn't seem like much, but in combination with the other measures listed above to improve your lifestyle, the effect can be quite significant.
Lifestyle improvement is warranted for almost all patients with hypertension, but drug treatment is indicated, although not always, in most cases.If patients with an increase in blood pressure of 2 and 3 degrees, as well as hypertension of any degree with a high calculated cardiovascular risk, drug treatment is mandatory (its long-term treatment(benefit has been demonstratedin numerous clinical studies), then in grade 1 hypertension with a calculated low to moderate cardiovascular risk, the benefit of such treatment has not been convincingly proven in large-scale clinical trials.In such situations, the possible benefit of drug treatment is assessed individually, taking into account the patient's preferences.If, despite the improvement in lifestyle, the increase in blood pressure in these patients persists for several months with repeated visits to the doctor, it is necessary to reassess the need for medication.In addition, the magnitude of the calculated risk often depends on the completeness of the patient's examination and may turn out to be significantly higher than initially thought.In almost all cases of hypertension treatment, they strive to stabilize blood pressure below 140/90 mmHg.Art.This does not mean that in 100% of measurements it will be lower than these values, but the lower the blood pressure, when measured under standard conditions (described in the "Diagnosis" section), exceeds this threshold, the better.Thanks to this treatment, the risk of cardiovascular complications is considerably reduced, and hypertensive crises, if they occur, are much less frequent than without treatment.Thanks to modern drugs, those negative processes that in hypertension inevitably and latently destroy internal organs (mainly the heart, brain and kidneys) over time, these processes are slowed down or suspended, and in some cases they can even be reversed.
Among the drugs intended for the treatment of hypertension, the main ones are 5 classes of drugs:
- diuretics (diuretics);
- calcium antagonists;
- angiotensin-converting enzyme inhibitors (names ending in -adj);
- angiotensin II receptor antagonists (names ending in -sartan);
- beta blockers.
Recently, the role of the first four classes of drugs in the treatment of hypertension has been particularly emphasized.Beta blockers are also used, but mainly when their use is required by concomitant diseases.In these cases, beta blockers serve a dual purpose.
Nowadays, preference is given to combinations of drugs, because treatment with one of them rarely leads to achieving the desired blood pressure level.There are also fixed combinations of medications that make treatment more convenient, since the patient only takes one tablet instead of two or even three.The selection of classes of drugs necessary for a particular patient, as well as their doses and frequency of administration, is carried out by the doctor, taking into account such data as the level of blood pressure, concomitant diseases, etc.
Thanks to the multifaceted positive effects of modern drugs, the treatment of hypertension involves not only lowering blood pressure as such, but also protecting internal organs from the negative effects of the processes that accompany high blood pressure.In addition, since the main goal of treatment is to minimize the risk of complications and increase life expectancy, it may be necessary to correct cholesterol levels in the blood, take medications that reduce the risk of blood clots (which lead to myocardial infarction or stroke), etc.So, treating hypertension involves tackling the disease in several ways, and achieving normal blood pressure is just one of them.
Forecast.Prevention
The overall prognosis is determined not only and not so much by the fact of high blood pressure, but by the number of risk factors for cardiovascular diseases, the degree of their severity and the duration of the negative impact.
These risk factors are:
- smoking;
- increased blood cholesterol levels;
- high blood pressure;
- obesity;
- sedentary lifestyle;
- age (with each decade lived after 40, the risk increases);
- male and others.
In this case, not only is the intensity of exposure to risk factors important (for example, smoking 20 cigarettes per day is arguably worse than 5 cigarettes, even though both are associated with a worse prognosis), but also the duration of their exposure.For people who do not yet have obvious cardiovascular diseases other than hypertension, the prognosis can be assessed using special electronic calculators, one of which takes into account gender, age, blood cholesterol level, blood pressure and smoking.The SCORE electronic calculator allows you to estimate the risk of death from cardiovascular disease over the next 10 years from the date of risk assessment.At the same time, the risk obtained in most cases, which is low in absolute figures, can give a misleading impression, because the calculator allows you to calculate the risk of cardiovascular death.The risk of non-fatal complications (myocardial infarction, stroke, angina, etc.) is several times higher.The presence of diabetes mellitus increases the risk compared to that calculated using a calculator: for men by 3 times, and for women - even by 5 times.
Regarding the prevention of hypertension, we can say that since the risk factors for its development are known (inactivity, excess weight, chronic stress, regular lack of sleep, alcohol abuse, increased consumption of table salt and others), then all lifestyle changes that reduce the impact of these factors also reduce the risk of developing hypertension.However, it is hardly possible to completely reduce this risk to zero - there are factors that do not depend on us at all or little: genetic characteristics, gender, age, social environment and some others.The problem is that people start thinking about the prevention of hypertension mainly when they are already in poor health and blood pressure is already increased to one degree or another.And it’s not so much a question of prevention as it is of treatment.

















